Oncology Note 6/29/24
Name:Fred Jones
Diagnosis:
CML-chronic phase
Prior Therapy:
Bone marrow biopsy done 12/28/2021-consistent with myeloproliferative disorder
Cytogenetics positive for t(9; 22) (q. 34; q. 11.2)
Ponatinib 45 mg: January 2023-present
Current Treatment/Plan:
Continue with ponatinib 45 mg daily
Reason for Clinic Visit: Follow Up
History of Present Illness: 45-year-old male who recently noted rash, increasing fatigue, some mental fogginess, occasional night sweats.
He was seen by his primary care provider, had labs done which revealed white count of 99,000, differential revealed segs, bands, metamyelocytes, promyelocytes, myelocytes and a rare blast. Patient underwent a bone marrow biopsy on 12/28/2021-findings consistent with a myeloproliferative disorder. Cytogenetics did reveal Philadelphia chromosome, translocation of chromosomes 9 and 22.
Interval History:
Fred is here for follow-up today.
BCR/ABL undetectable.
Side effects are unchanged and include fatigue and occasional constipation. These are manageable.
He denies any fever, chills, night sweats, unintentional weight loss, lymphadenopathy, n/v, diarrhea, chest pain, or SOB.
Review of Systems:
A 10-point review of systems was assessed; all systems were negative except per Interval History.
Pertinent History:
Past Medical History
Diagnosis
o Acne vulgaris
o Anxiety
o Chronic low back pain
o CML (chronic myelogenous leukemia)
o History of DVT (deep vein thrombosis)
o History of gout,
o History of left THA (total hip arthroplasty)
o History of tonsillectomy
o Hypercholesterolemia
o Hypertension
o Obesity
o OSA (obstructive sleep apnea) on CPAP
o Seasonal allergies
o Type II DM (diabetes mellitus)
Past Surgical History
TOTAL HIP ARTHROPLASTY Left 5/2022
TONSILLECTOMY 1985
Pertinent family history includes Breast Cancer (age of onset: 60) in his maternal grandmother; Cancer in his maternal grandmother and mother.
Current Outpatient Medications:
· Atorvastatin 20 mg daily
· Aspirin 81 mg daily
· Ponatinib 45 mg daily
· Metformin 1000 mg BID
· Glipizide 5 mg daily
· Lisinopril 20 mg daily
Review of patient’s allergies indicates:
o Allopurinol - Rash
Objective:
Vitals
· Height: 6' 0" (1.828 m)
· Weight: 310 lbs (140.6 kg)
· BP: 113/75
· Temp: 97.3 °F (36.3 °C)
· Pulse: 62
· Resp: 16
Physical Exam:
General: Alert and oriented, pleasant, appears in no acute distress.
Skin: Warm and dry, no rash. Skin tone appropriate for race.
HEENT: No icterus. No conjunctival injection or discharge.
Neck: Soft and supple, no cervical, supraclavicular lymphadenopathy.
Lungs: Clear to auscultation bilaterally, no wheezes, rhonchi, or rales. Breathing non labored.
Heart: Regular rate and rhythm.
Abdomen: Soft and nontender to palpation. No axillary adenopathy.
Extremities: No edema.
Musculoskeletal: Steady gait, changes positions easily.
Psych: Mood and affect appropriate.
Laboratory
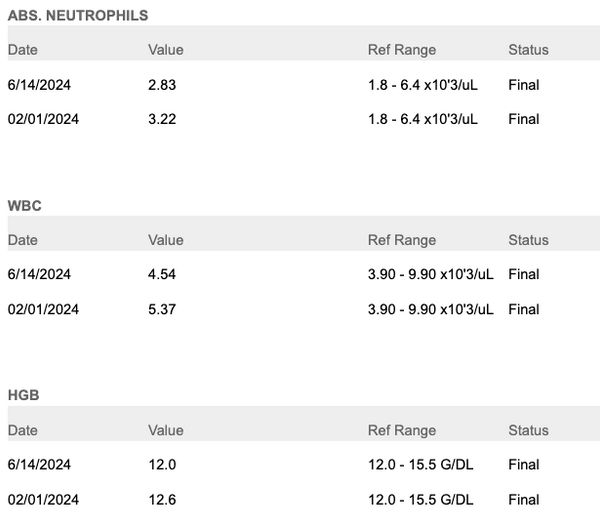
CBC:
CMP:
Tumor Markers:
Assessment and Plan
1. CML
-CBC, CMP, and BCR/ABL reviewed. BCR/ABL remains undetectable.
-Continue with ponatinib 45 mg daily.
-Labs/exam with BCR/ABL in 6 months
FOLLOW UP: RTC in 6 months for next BCR/ABL quantitative check. Pt advised to call with any new or concerning symptoms.
I spent 25 minutes today reviewing the patient's medical record, obtaining history, documenting in the medical record, counseling and educating the patient, and reviewing and communicating test results
Dr. Cure